
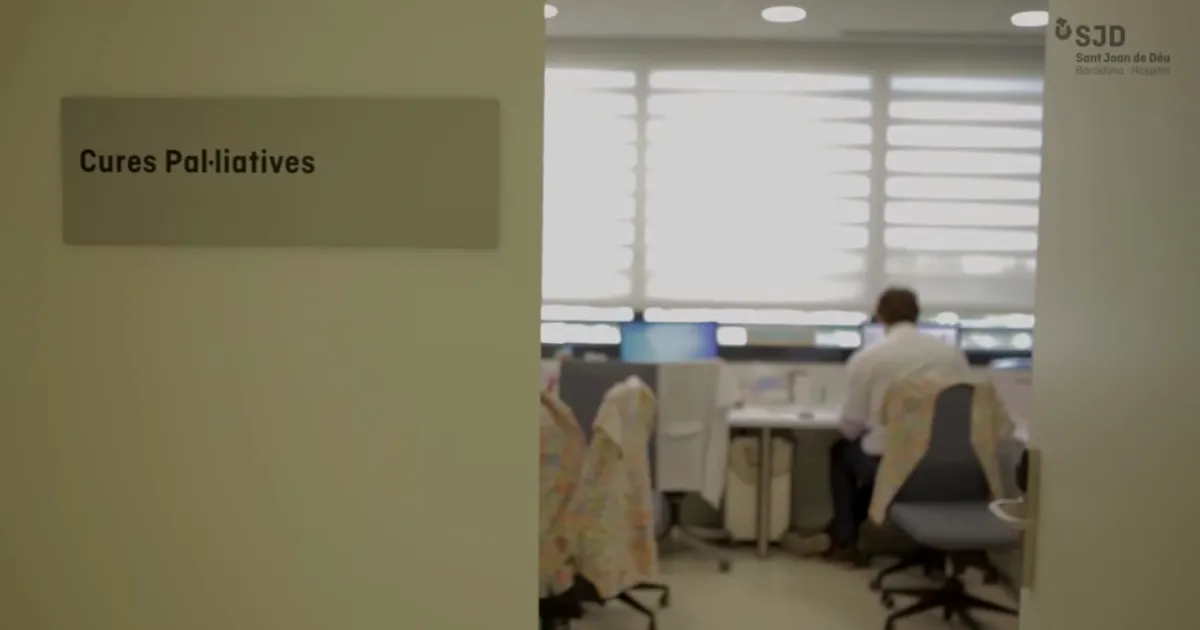
In the Palliative Care and Chronic Complex Patients department, we provide care for children and teenagers with severe diseases, and also offer emotional support to their family.
We provide ongoing comprehensive care to children with severe diseases who likely will not reach adulthood, as well as to their families. We consider parent and child as inseparable when aiming to provide comprehensive care.
In such situations, patients often have several, complex requirements. The team's goal is to provide physical, social, emotional and spiritual support. While one of the main functions of our team is to help manage the symptoms that can arise with complex diseases, our primary goal is to ensure the child and family's well-being.
The Palliative Care and Chronic Complex Patients team is made up of two pediatricians, four nurses, a social worker, a spiritual counsellor and a psychologist, all specialised in pediatric palliative care. All of these professionals are necessary to providing the comprehensive care we strive for, as when a patient is diagnosed with a severe illness, all aspects of the child and family's life are affected. Keeping in mind the complexity of their work, we as an institution look after our professionals as much as possible so that they can provide optimal care.
Why the SJD Barcelona Children's Hospital?
Our Palliative Care and Chronic Complex Patients unit is one of the most experienced in Spain.
We are innovators and experts
We are one of the most experienced units in palliative care and complex chronic patients in Spain.
- We started in 1991 and we were the first Paediatric Palliative Care unit in Spain.
- Since 2009, we have cared for more than 587 patients and their families.
We provide comprehensive, customised care that is adapted to the needs of the child and their family.
Continuing care wherever patients are
We offer comprehensive and personalized care adapted to the needs of the child and his family.
- We offer hospital-level outpatient and hospital-at-home care. Care can be focused according to the needs of the child and his/her family.
- There is a 24-hour telephone service to deal with emergencies and questions at any time of day or night, every day of the week, including holidays. In some cases a doctor and/or nurse may be able to come in-person to where the child and his or her family are.
We are there to provide emotional support at all stages of a disease.
We support families
We offer accompaniment and emotional support in all phases of the disease
- Another function of the service is to train families so that they can carry out the necessary care at home. This is about giving carers the tools they need to take the proper action and deal effectively with different situations, always with the support of the Palliative Care and Complex Chronic Patient Unit's professional team.
- This also involves training carers so that they can control the symptoms of the disease and help them to address the family's situation, both practically and emotionally. We help them to assess when and how to give information, such as talking to siblings if there are any, as well as to the patient.
- We offer emotional support and follow-up during mourning.
Our work method is based on cross-departmental relationships with other areas of the Hospital.
Teamwork
Our working method is based on the interrelationship and coordination with other hospital departments
- Together, all the professionals involved form one team. We implement a treatment plan with all the professionals of the units involved in a patient's care. The plan is agreed on by the referring team and the family. It contains the objectives to be met, the family's strengths, problems that may arise and how to solve them.
- We have also established links with primary care and other teams, such as PADES (Home Care Programme and Support Teams). The interdisciplinary team can establish channels of communication with other systems besides healthcare (social services, educational system, etc.).
- Admission to the Palliative Care and Complex Chronic Patient Service does not necessarily entail a change in the patient's treatment or testing. In other words, patients will continue going to see their specialist at the hospital as required. Clinical or lab tests may be able to be done by the team at a patient's home, thus avoiding disruptions to the family's normal routine and the inconvenience of having to travel to the hospital.
La Casa de Sofía is the first care facility for children with rare and chronic, complex diseases
The Palliative Care and Chronic Complex Patients team leads this facility, whose goal is to avoid or delay the hospitalisation of children with advanced disease or chronic complex illnesses.

Team
‘Our team eases suffering and improves quality of life for children with life-threatening severe illnesses’







- Begoña Magriña, psychologist at the Fundación Paliaclinic.
- Verónica Gimeno Alcalá, nurse.
- Marta Viñals Miralles, psychologist.
- Georgina Morón Cazalilla, paediatrician.
- Nuria Rayo Monreal, nurse.
- Mar Sánchez Ruiz, nurse.
- Alba Giró Subirats, project manager.
- Lourdes Mayo Tejeda, secretary.
- Alex Torné Cortes, office clerk.
- Giuliano Varriale, clinical assistant.
Palliative care made caring for our daughter easier in every sense
Information for families
From birth and through infancy and adolescence, children can develop severe illnesses that reduce their life expectancy or that come with side effects that can threaten their survival.
Despite scientific and medical advancements, some children also sadly pass away in our care. These children with severe diseases go through a long process with many different stages, which impacts the lives of everyone around them, flipping their world upside down.
Any process involves several stages, which in this case would be the following:
Stage 1: Diagnosis
If your child is going through these circumstances, it is likely that the first hurdle has been coping with diagnosis. Or possibly the lack thereof. It's not always easy to put a name to a disease.
At times, despite all efforts, a definitive diagnosis is never reached.
Stage 2: Treatment
The goal in this stage is to find and provide the best treatment possible for your child. At the SJD Barcelona Children's Hospital, we are always carrying out new kinds of treatments, and our specialists are in touch with professionals all over the world to try to find new alternatives that could help each child.
This stage can last a long time. You, your child, your family… you will all be in a set of very vulnerable, fragile, complicated circumstances which can affect you in several ways, be that physically, emotionally, socially, economically and/or spiritually.
This situation requires the involvement from various disciplines, both medical and other. Whether it is at our Hospital or another, we must always try to provide what is needed.
It is not always possible to offer curative treatment. At this point, the goal becomes prolonging life, often for years, in the best, most dignified way possible.
Stage 3: Palliative Care
This type of care follows a comprehensive, integrated and integrative model to ensure all needs are met.
The team in the Palliative Care and Chronic Complex Patients Department at the SJD Barcelona Children's Hospital is made up of pediatricians, nurses, a social worker, a psychologist and a spiritual counsellor. Working together, and with the involvement and input of all team members, we are able to address the needs of each child on an individual basis, always keeping in mind their story and circumstances.
We wholeheartedly believe that all children with a life-threatening or life-shortening disease, as well as their family, should receive palliative care from first diagnosis.
FAQs
We understand that it can feel confusing when your doctor offers your child follow-up with the Palliative Care and Chronic Complex Patients Department.
However, please remember that whether your child receives palliative care or not, it does not necessarily change the disease's outlook, nor does it change the goals of the medical team that has treated your child so far. The only things that can change our clinical goals are how the disease progresses and the child and family’s wishes.
It is very important that you know why this specific point during the disease has been chosen to start palliative care, so do not hesitate to ask questions if you have not yet been told.
There can be several reasons, such as:
- Perhaps your child’s symptoms are becoming difficult to manage, their disease has progressed and there are expected to be short-mid-term complications.
- Care could be provided at home instead, meaning you do not need to come to hospital as much.
The reality is that the Palliative Care team knows about your child's case basically since diagnosis. But their job at that point is to assess the disease and assist the specialist you have been dealing with so far.
The fact you now know of us is because the situation has become more complex. Our involvement is of better benefit to you now than before, and we can help respond to new needs that have arisen due to the disease's progression.
Severe diseases often require aggressive treatments that can cause pain and other symptoms. They can lead to discomfort and suffering, but we can anticipate these symptoms and try to properly manage them with palliative care, therefore minimising their impact.
That is why it is essential to complement curative, targeted treatments for the disease with palliative care, which is meant to ease the symptoms.
Receiving palliative care does not mean withdrawing or limiting treatment. In fact, measures that can be implemented can be short-term and even help improve the disease.
If curing your child’s disease is not possible, the goal could be to stabilise or delay its progression, thus helping daily life feel more normal and improving overall quality of life as much as possible.
Coming and going to the hospital with your child can feel never-ending. Spending hours in waiting rooms and appointments with lots of different specialists can become routine for families. Even being admitted to a hospital ward can feel like just another day.
When the disease progresses to a point where your child requires a greater degree of care, this can mean spending more time in hospital.
Our experience has shown that stress is reduced for the whole family if problems can be addressed at home.
In their last days of life, severely ill children often want to be at home, with their toys, in their room, with siblings if they have them, and with the rest of the family. Our team does everything we can to fulfil these wishes, supporting parents throughout the whole process.
As such, parents will have more time for other tasks, such as running the household, work, or looking after other children. And all of this, while providing the same level of care your child would receive in hospital.
Depending on your child's situation, our team can administer the same treatments at home as they do in the hospital environment. What actually changes is that we put the child's comfort above clinical results. The goal is no longer to cure, but rather to achieve the highest quality of life.
It is normal to feel afraid or uncertain when thinking about caring for your child at home until the very end. Our team will help you, explaining what can happen and showing you how to manage the medication and care that your child will need. You will also have a 24-hour phone helpline that you can call at any time for anything you need.
It is impossible to know exactly how long anyone will live. It is the same with children: each child is unique and responds differently to the same situation. But we can base our estimations on your child’s progress and symptoms to figure out when they are approaching the end. Decision-making can be hard here, but we will be by your side just like we have been every step of the way.
There can sometimes be treatments that do not provide any benefit, or that even cause more harm than good. In these situations, we must focus on what is better or worse for your child, to ensure their quality of life is as high as possible.
The harder a disease is to cure and the more severe it is, the more important family becomes: each family is unique, with their own values and stories. This means that healthcare staff may ask you whether the measures being implemented for your child align with your family values or not.
The Palliative Care and Chronic Complex Patients Department seeks to provide families with the tools they need so that this difficult, tragic situation does not become overwhelming, and therefore minimise the suffering that comes with it. We will help you to come together as a family to get through these difficult moments.
In addition, families have other needs—whether financial, caring for other children or sick relatives, or work—that make caring and being there for their sick child during their illness more difficult. The Palliative Care and Chronic Complex Patients Department can perform an analysis of what kind of resources (both personal and material) you may need, and help you as much as possible.
‘Thank you for being there for us on this long journey, for making our lives easier and for helping us to accept the unacceptable. In these painful, difficult moments for our family, having been able to count on your help, your support and your knowledge, is something we can never repay and certainly never forget.’ - Testimonial from L.B.
‘In the at-home visits and regular phone calls we were given advice, encouragement and comfort. They were always there when we needed them, for whatever emergency. We only have good things to say about these professionals who have supported us and our son on this complicated journey that he unfortunately had to face. It would have been impossible to do all of this from home without their help’ - Testimonial from M.C.
‘For us, the palliative care team do a fantastic job, one that not everyone is able to do. They stand out for many good reasons: altruism, solidarity, empathy, strength, commitment, company, warmth, generosity, and so much more. We have been through tough times, and despite the challenges, we have learned and been taught so much. But if we are left with anything, a small detail, a moment, a virtue, it's that they were always there when we needed them.’ - Testimonial from E.R.
‘You helped make everything easier. We could relax at home because we knew that we could call you anytime and at the other end of the phone would be a friendly, professional, and above all, compassionate voice with whom we could share our fears in complete confidence, and that the answers and care we’d be given would be the best for our child and us. [...] Thank you for letting us have precious moments with our son’. - Testimonial from F.A.
Resources for families
Summary of the care criteria document for Pediatric Palliative Care from the Department of Health, Social Services and Equality.
NGDO that helps improve Palliative Care (PC) and Pain Relief (PR) in Latin America and Africa.
Palliative care is a comprehensive care approach for mind, body and spirit of the child, as well as support for the family. This care begins when a life-threatening disease is diagnosed and continues regardless of whether the child receives treatment for the disease or not.
Research
The Institut de Recerca Sant Joan de Déu (IRSJD) boasts a research group into Chronicity and pediatric palliative care, whose aim is to increase knowledge of complex chronicity and pediatric palliative care, thereby improving the care offered to these patients and their families.
Teaching
We have been pioneers in paediatric palliative care since 1991. We train professionals so that they can guarantee the well-being of children with serious incurable illnesses and their families, through a comprehensive care model and in coordination with other hospital services and local resources.











