At BCNatal - SJD Barcelona Children's Hospital we are specialists in the treatment of congenital diaphragmatic hernia and in precise fetal surgery for its treatment. We have a comprehensive congenital diaphragmatic hernia (CDH) treatment program with which we treat an average of 18 patients per year. Our care includes medical care, surgery and follow-up until school age.
Description
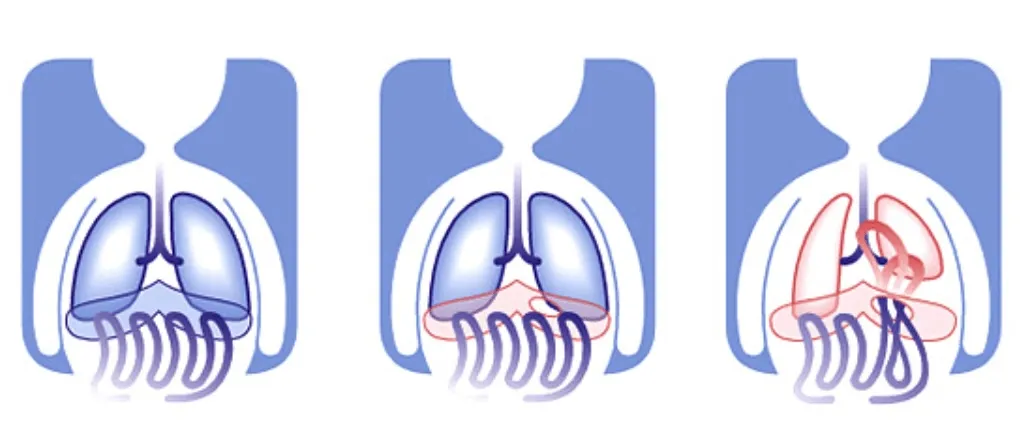
Congenital diaphragmatic hernia (CDH) occurs in approximately 1 in 2500 pregnancies. It is a defect in the fetus' diaphragm, a thin muscle resembling a very large disc that completely separates the chest (where the lungs are located) from the abdomen (where the stomach, intestines and liver are located). In CDH, the diaphragm has a hole because it did not completely close during fetal development.
When a CDH is present, the organs in the abdomen (stomach, intestines and liver) can ascend to the chest through the diaphragm hole and compress the lungs. If this occurs, the lungs of the fetus cannot grow and develop normally due to lack of space (pulmonary hypoplasia), which can cause serious breathing problems at birth, even leading to the death of the baby.
Diagram of congenital diaphragmatic hernia (CDH)
Why does it occur?
The cause of CDH is unknown and can occur in several forms, such as a genetic syndrome or associated with other malformations. However, in more than half of cases it presents as an isolated disease with no other problems.
What kind of problem does it represent?
During intrauterine life, the fetus does not use the lungs to breathe; rather, the blood is oxygenated by the placenta. Therefore, in many cases of CDH the baby will be able to have surgery after birth.
However, in more severe cases, the lungs may be too small (severe pulmonary hypoplasia) to be able to breathe after birth, and despite treatment the baby will develop respiratory failure and will not be able to survive. The same can happen with the blood vessels of the lungs, causing problems in the blood circulation to the baby through the lungs (pulmonary hypertension).
The risk in each case can be very variable. In some babies the hole in the diaphragm is small, they need little help breathing and their chances of survival are very high. In others, the defect can be very large, needing a lot of help and leading to low chances of survival.
Each case may be different, but CDH is always a serious disease that will need a lot of care in the first few months of life. For this reason, babies with CDH should always be born in a third-level hospital with highly specialized staff and extensive experience in the management of such cases.
Medical diagnosis
The probability of a better or worse outcome will depend on the degree of pulmonary hypoplasia, that is, how small the lungs of the fetus are. In those cases with a worse prognosis, prenatal (before birth) therapy by fetal surgery may be considered, which could greatly increase the chances of survival.
Once the diagnosis has been made, a comprehensive evaluation by an experienced fetal medicine team is essential, which will assess whether it is an isolated case of CDH or if there are other added problems. To this end, a series of studies and different assessments are carried out:
- Specialized ultrasound to calculate the size of the lungs and know the viscera that are herniated into the chest; the liver is especially important.
- Amniocentesis and genetic study to know if CDH is associated with other genetic abnormalities and to rule out that it is an isolated CDH.
- MRI to obtain a comprehensive view of the fetus that will be used, if necessary, to support surgery.
- Multidisciplinary assessment involving fetal medicine specialists, neonatologists and paediatric surgeons.
Once the study is complete, we can establish a fairly accurate forecast of survival chances. In general, when the probability of survival at birth is less than 60%, fetal surgery is offered, that is, a treatment that is applied before birth to reduce the lung damage that occurs throughout pregnancy.
Treatment
Once the study to determine the prognosis is completed, the situation is discussed in detail with the parents, who always have the final say on the treatment in each case:
- Conventional treatment at birth: this consists of giving respiratory support immediately after birth with medication and help with various types of assisted breathing until the diaphragm hole can be repaired. It involves repositioning the abdominal organs in place and closing the diaphragm defect, with the intention that the lungs can expand and perform their breathing function.
- Treatment by fetal surgery (fetoscopic tracheal occlusion or FETO): this is a procedure to temporarily close the trachea (the tube through which we breathe, which goes from the throat to the lungs), not with the aim of repairing the hernia but to increase lung growth and give the baby maximum options when it is born. In such cases, conventional treatment and repair of CDH at birth is also necessary.
What is fetoscopic tracheal occlusion (FETO)?
This fetal surgery treatment aims to try to stimulate the growth and development of the lungs before birth, to increase the chances of survival. Its purpose is not the repair of the defect of the diaphragm since this must be closed by surgery after birth. This prenatal therapy can substantially increase the chances of survival in cases with a worse prognosis.
Like any other fetal therapy, treatment carries some risks. In addition to requiring the admission of the pregnant woman, it slightly increases the risk of preterm birth. For this reason it is only offered when it is estimated that the chances of survival with a conventional treatment are less than 60%. The most recent results suggest that treatment may increase the probability of survival by 30-40% compared with that initially calculated.
Treatment is performed at around 30 weeks of pregnancy by fetal endoscopy (fetoscopy). It consists of obstructing the trachea of the fetus with a kind of balloon. This blockage does not let out the fluid produced by the lungs of the fetus and causes it to grow a higher rate.
In addition, tracheal occlusion causes the lung to "inflate" and counteract the pressure it is suffering from the stomach, liver, or intestines that have risen to the fetal chest. It is this accelerated growth of the lungs that will give the baby many more options when it is born.
Fetoscopy is a minimally invasive therapy, so the pregnant woman is usually hospitalized for 1-2 days. It is performed in the operating theatre, almost always with local anaesthesia, since only a small cut, of about 3 mm, in the abdomen of the pregnant woman is necessary. Through this hole a small tube (fetoscope) is inserted into the uterus and through the mouth of the fetus to the trachea, where the balloon is inflated.
This is left inflated for a period that can range from two to four weeks, to be removed later in a second admission with a similar operation. Once removed, the pregnancy is monitored frequently and in most cases the baby can be born vaginally.
What appointments are needed for fetal surgery?
An in-patient admission of the pregnant woman will initially last 1–2 days and afterwards weekly check-ups with examination and ultrasound will be required, and she will have to maintain a low-activity lifestyle mainly at home until the end of pregnancy, especially for the first 3-4 weeks after the intervention. It is essential that between the first and second fetoscopies, for the placement and for the subsequent removal of the balloon, the patient remains near the hospital (within a distance it would take less than 1–2 hours to travel). Normally, pregnancy can continue to term without the need to induce birth prematurely.
During pregnancy, you will receive the support of nurses specialized in fetal medicine, not only on a technical level but also on an emotional level throughout the process. In addition, we can put you in contact with other families who have gone through the same experience. This experience is very positive and helps to humanize and understand the problem in a much more intuitive way and without the difficulties that sometimes arise when receiving only technical information from professionals.
Why BCNatal - Sant Joan de Déu?
In short, for parents who want to continue their pregnancy care and have their baby with us, we offer a team of fetal and paediatric surgery and neonatology with the most experience, and the best survival figures and quality of life that can currently be obtained.
We are pioneers in the prenatal treatment of congenital diaphragmatic hernia (CDH) by fetal surgery (fetoscopic tracheal occlusion or FETO).
Our experience and effectiveness
We are pioneers in the prenatal treatment of congenital diaphragmatic hernia (CDH) by fetal surgery (fetoscopic tracheal occlusion or FETO).
- Dr Eduard Gratacós was part of the team of specialists that designed and used the current technique for the first time in the world.
- We have performed more than 300 fetal CDH surgeries, being one of the centres in the world with the most experience in the evaluation and treatment of CDH.
- CDH is a serious disease that requires a lot of care in the first months of life. For this reason, fetuses with CDH should always be born in a third-level hospital as SJD Barcelona Children's Hospital, with highly specialized staff and extensive experience in the management of such cases.
- Despite its technical difficulty and that it requires substantial preparation and planning, the actual duration of the operation (from the time the endoscope is inserted into the uterus until it is removed) is usually not more than 10 minutes in our experience. This means that the risks of added prematurity, rupture of membranes and infection (possible complications of fetal surgery) are very low today compared with those of 15 years ago when treatment was started and less experience was available.
Fetal surgery for CDH is offered in a small number of hospitals around the world. It is a complex, delicate and very precise treatment, since the surgeon inserts a small tube of 2 to 3 mm into the trachea of the fetus. However, in expert hands it is a very non-aggressive treatment for the pregnant woman and the fetus. In fact, no incision is made to the fetus since the mouth is used to introduce the balloon.
We are a multidisciplinary team, which allows us to approach surgery in a comprehensive way: from the choice of the best strategy to individualized postnatal follow-up.
Highly specialized team
We are a multidisciplinary team, which allows us to approach surgery in a comprehensive way, from the choice of the best strategy to individualized postnatal follow-up.
A la excelencia del equipo prenatal se suma un centro pediátrico de tercer nivel con gran número de especialistas en cuidados intensivos neonatales y la mejor y más moderna tecnología. Esto permite disponer todos los días del año, a cualquier hora del día, de profesionales médicos y de enfermería altamente cualificados en el cuidado de estos delicados pacientes. Este aspecto es muy importante porque el tratamiento postnatal de la HDC es muy complicado y la enfermedad es poco frecuente, lo cual dificulta adquirir experiencia. Desde hace casi 20 años, gracias a nuestro programa de cirugía fetal, nuestro Servicio de Neonatología atiende un número de casos de HDC muy superior a la media de otros hospitales y cuentan con una de las mayores experiencias en Europa.
Una vez dado de alta, los equipos de Pediatría seguirán al bebé durante los primeros meses, y años después, para conseguir el mejor desarrollo y avanzarse a cualquier problema en esta parte tan fundamental de la vida.
As a pioneering development centre, we continuously research and incorporate technologies that further improve accuracy.


