We are specialists in the treatment and in the precise fetal surgery of fetal tumors of the face and neck.
Pathology description
What are fetal tumours of the neck and face?
The most common large tumours of the fetal face and/or neck are cervical teratoma and lymphangioma, their origin being often the structures of the mouth (tongue, gums, pharynx) or fetal thyroid. They are almost always benign tumours, not cancer, and in most cases they have very good treatment options after birth.
The main problem during fetal life is that they can grow to such large proportions that the fetal airways become distorted and clogged and the newborn cannot breathe. In addition to clogging the airways, they can also compress the oesophagus (the digestive tract that runs from the throat to the stomach), resulting in an excess amount of amniotic fluid (polyhydramnios) that can cause a premature birth.
Why do they occur?
Unfortunately, we do not know what causes large tumours of the face and/or neck. However, we do know that they are not a genetic problem and, therefore, that they are not hereditary.
What kind of problems do they represent?
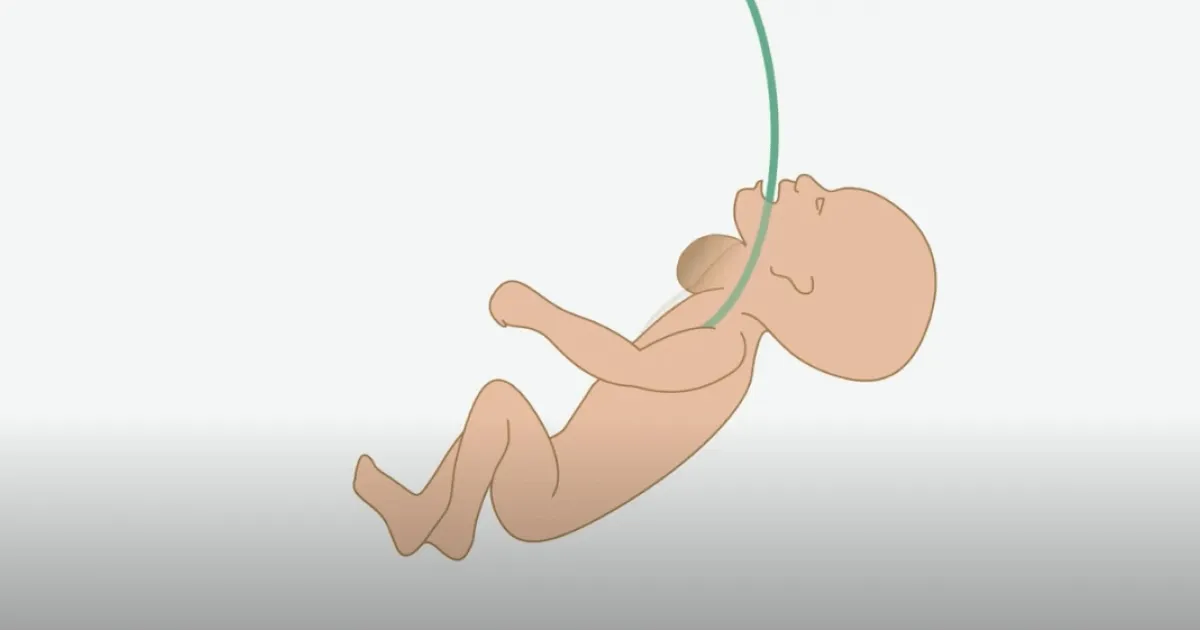
Before birth, the fetus receives oxygen and nutrients through the placenta. Oxygen from the placenta reaches the fetus through its umbilical cord, so it does not need to use its lungs before birth. Once the baby is born and takes its first breath, the lungs begin to function and the placenta is no longer required as a source of oxygen. Usually, the placenta is detached with the first contractions following the birth of the baby and then removed.
In the case of tumours in the face or neck, these can clog the fetal airways, such as the larynx or trachea (the tubes that connect the mouth to the lungs and through which we breathe). When this occurs, the baby is fine until delivery because the placenta fulfils the function of the lungs. But when the baby is born and tries to breathe for the first time, it cannot fill its lungs with air. When the placenta detaches, the baby has no way to take oxygen into his or her body and requires emergency measures to stay alive.
Explanatory video of BCNatal fetal surgeries for face and neck tumors
Diagnostic
Once the diagnosis has been made, a comprehensive evaluation by an experienced fetal medicine team is essential, which will assess if it is an isolated pathology or if there are other added problems. To this end, a series of studies and different assessments are carried out:
- Ultrasound and echocardiography to calculate the size of the lungs and assess cardiac function.
- Amniocentesis and genetic study to know whether the tumour is associated with genetic abnormalities.
- Magnetic resonance imaging to obtain a comprehensive view of the fetus that will be used, if necessary, to support the surgery, facilitating its planning and minimizing the associated risks.
- Multidisciplinary assessment involving fetal medicine specialists, neonatologists and paediatric surgeons.
Treatment
In the case of tumours of the face or neck that compress and distort the airways of the fetus, the indicated treatment is the EXIT procedure (ex utero intrapartum treatment).
This procedure is a maternal-fetal surgery technique that allows the maintenance of the circulation, and therefore oxygen, between the pregnant woman's uterus and the placenta while carrying out the necessary interventions (an orthotracheal intubation or a tracheostomy) in the baby's airway so that the baby can breathe after birth. It is also used to resect cervical or thoracic tumours.
The EXIT procedure is performed during an elective (pre-scheduled) caesarean section before separation of the placenta. It is necessary to have a multidisciplinary team with high experience in performing fetal and neonatal surgery. The coordination of the team is essential to achieve excellent results for both the pregnant woman and the baby during an EXIT caesarean section.
What complications can the EXIT procedure have?
Although it is a very established surgery, it must be performed by expert teams since there are risks and potentially serious complications for the pregnant woman and the fetus, such as:
- Risk of lack of uterine contractility and, as a result, severe postpartum haemorrhage. This can occur due to the necessary relaxation of the pregnant woman's uterus to keep the placenta unsealed and thus able to oxygenate the fetal blood through the circulation between the uterus and the placenta.
- Risk of uterine rupture in subsequent pregnancies, if incisions have been used in the uterus that are not typical of caesarean section (transverse and low) during the procedure.
- Fetal complications related to lack of oxygen due to failure to maintain the exchange between uterus and placenta due to cord compression or placental abruption.
- Complications related to the basic pathology of the fetus.
What controls should I do in case of EXIT fetal surgery?
We will perform weekly check-ups with examination and ultrasound, to monitor the size of the tumour and rule out the development of excess amniotic fluid (polyhydramnios) that could cause a premature birth. Similarly, the pregnant woman must maintain a low-activity lifestyle mainly at home until the end of pregnancy. Typically, the EXIT intervention can be performed between 34 and 37 weeks of gestation.
During pregnancy, you will receive the support of nurses specialized in fetal medicine, not only on a technical level but also on an emotional level throughout the process. In addition, we can put you in contact with other families who have gone through the same experience. This is very positive and helps to humanize and understand the problem in a much more intuitive way and without the difficulties that sometimes arise when receiving only technical information from professionals.
Why SJD Barcelona Children's Hospital?
For parents who want to continue their pregnancy care and have their baby with us, we offer a fetal surgery team with the best survival figures and quality of life that can currently be obtained.
We have one of the world's largest experiences in fetal surgery, with more than 2000 interventions performed, the shortest surgical times reported in the medical literature and, consequently, very low rates of complication.
Experience and efficiency
We have one of the world's largest experiences in fetal surgery, with more than 2000 interventions performed, the shortest surgical times reported in the medical literature and, consequently, very low rates of complication.
- Dr. Eduard Gratacós performed the first EXIT surgery in Spain more than 20 years ago, and since then we have performed a significant number of these interventions, being one of the most experienced international groups.
- As a pioneering development centre in fetal surgery, we continuously research and incorporate technologies that further improve accuracy during surgery.
- Through a pioneering three-dimensional simulation system, we can visualize and print 3D models that allow us to simulate and practice the intervention before performing it, minimizing the surgical time required and the associated risks.
We are a multidisciplinary team, which allows us to approach surgery in a comprehensive way.
Personalized patient-centered care
We are a multidisciplinary team, which allows us to approach surgery in a comprehensive way
Before surgery we evaluate each case in detail, performing very high-resolution ultrasound and magnetic resonance tests, and perform analysis in multidisciplinary teams that include experts in each of the fields, including fetal medicine, fetal and pediatric surgery, otoraryngologists, neonatologists, radiologists and any other specialty that may be necessary.
We will discuss the case in detail with the parents and talk about the best options for your baby. Parents will be able to speak in detail not only with specialists in medicine and fetal surgery, but also with pediatricians who are experts in the monitoring and evolution of these children, to get to know in detail the expected evolution in each case and the best options.
We accompany you with an individualized postnatal follow-up.
After the birth we continue with our patients
We accompany you with an individualized postnatal follow-up
To the excellence of the prenatal team is added a third-level pediatric centre, as SJD Barcelona Children's Hospital, with teams made up of a large number of specialists with specific training in neonatal intensive care, and who have the best and most modern technology. Paediatric surgeons, also part of the prenatal team, will continue to care for the baby once it is born and plan for possible interventions as needed. The most common specialists are otolaryngologists and pediatric surgeons. For surveillance during the first days after birth, the hospital has highly qualified medical and nursing professionals caring for these delicate patients 24 hours a day, 365 days a year.
Once discharged, our paediatric cardiology teams will follow the baby for the first few years and take care of him or her to achieve optimal development and to solve any problems in this very fundamental part of life.
